Actinic Keratoses
Actinic Keratoses (AK) are also referred to as solar keratoses - they are considered 'precancerous' lesions that have the potential to progress into invasive SCC; the estimates of progression vary from a rate of 0.075-0.1% per lesion per year to ~10% over 10 years. They commonly appear on sun-exposed areas of the skin individuals with a history of cumulative sun exposure. It may present with irregular, red, scaly papules or plaques on sun-exposed regions of the body. Timely detection and treatment is crucial since the risk of progression to SCC is present.
Etiology
AKs are usually the result of cumulative effects of UV radiation on the skin that occur over an individual's life.
Epidemiology
AKs predominantly appear on chronically sun-exposed body areas, in older individuals who have decades of sun exposure. Common locations include:
Face
Scalp
Back of the arms
Dorsal aspect of the hands
Risk factors that may contribute to the development of AK is influenced by increased age, male gender, fair-skinned individuals (Fitzpatrick skin phototypes I and II), geographic location, immunosuppression (AIDS, organ transplant, leukemia), history of AKs or previous skin malignancy and excessive/chronic sun exposure.
Pathophysiology
Excessive/cumulative UV exposure can trigger pathological changes in the epidermal keratinocytes by disrupting regulatory pathways involved in cell growth and differentiation. This disruption leads to inflammation and immunosuppression, contributing to the proliferation of dysplastic keratinocytes, the precursors of actinic keratosis.
Histopathology
Presence of atypical keratinocytes within sun-damaged skin that is limited to the lower third of the epidermis
Presentation and History
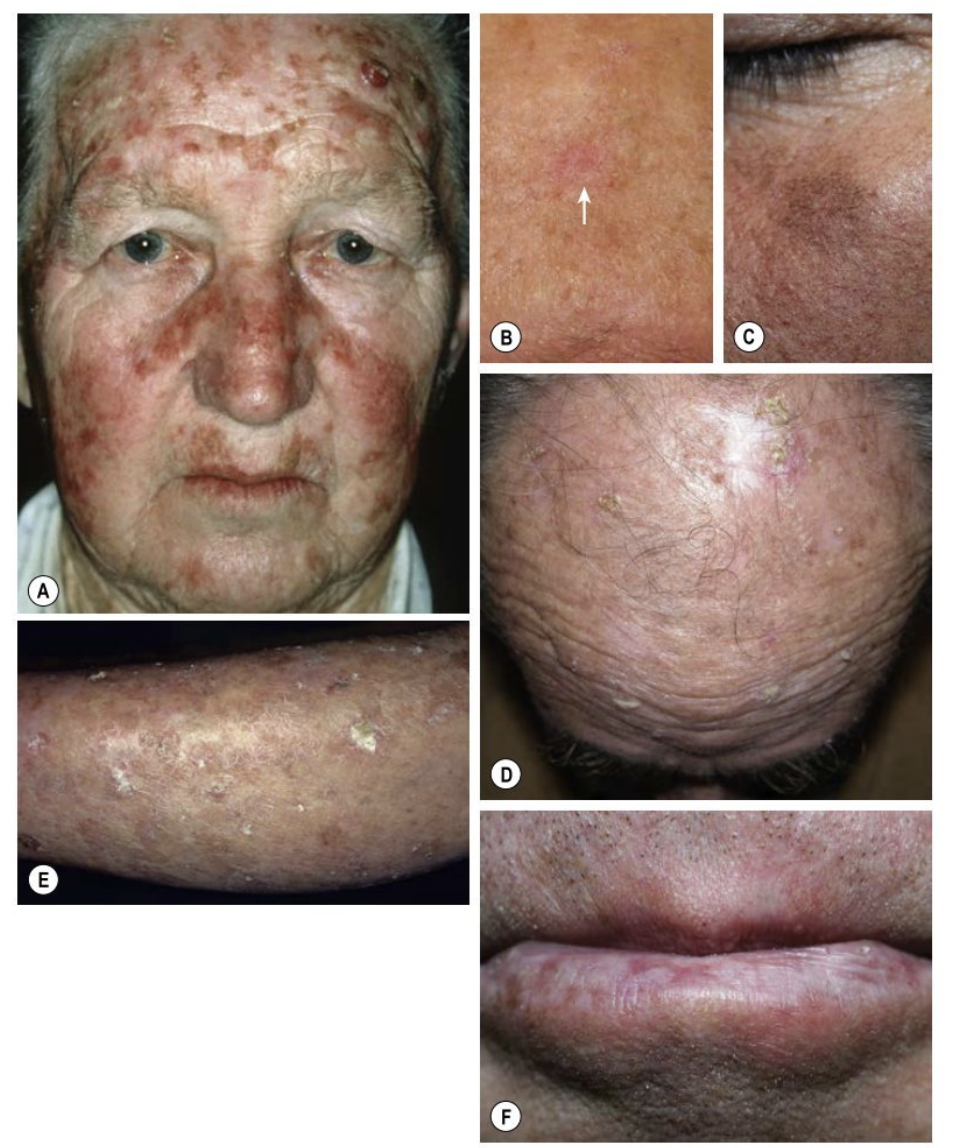
The classic presentation is a graitty papule with an erythematous base; the associated scale is usually white to yellow in color and feels rough (figure A). There are common clinical variants:
Pigmented: Figure C
Hypertrophic (HAK): Figure D and E
Lichenoid and atrophic: Figure B
Actinic cheilitis: Scaling of the lower vermilion lip (Image F)
AKs presenting symptoms are typically asymptomatic, but there are certain symptoms that may indicate an increased risk of invasive squamous cell carcinoma progression:
Pruritus (itching)
Pain or ulceration
Bleeding with minor trauma
Investigation and Diagnosis
Diagnosis is based on clinical observations. However, additional diagnostic techniques such as dermoscopy or biopsy may provide valuable information in certain cases. Dermoscopy can reveal characteristic features such as a 'strawberry pattern' in nonpigmented facial AK. This pattern includes an erythematous vessel pseudo network, prominent follicular openings, and a surrounding white halo.
In certain circumstances, a biopsy may be necessary to confirm the diagnosis of AK. A biopsy is reserved for individuals who fail to respond to treatment or in situations where one wants to determine if an AK has progressed to a squamous cell carcinoma.